views
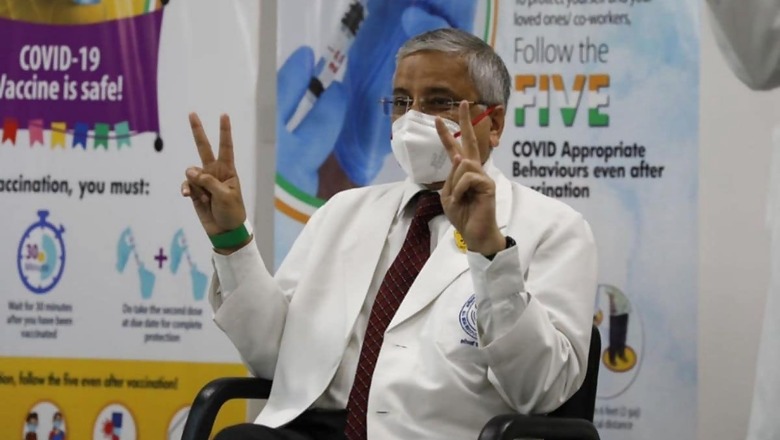
The destructive second wave of the Covid-19 pandemic that is sweeping through vast swathes of India right now has brought with it unimaginable carnage and misery. It has also brought with it questions. Millions of Indians are trying to come to terms with the gloomy situation around and are trying to understand the reasons behind the calamitous return of the pandemic, the many variants fuelling the spread, the ways to stay protected, the merits of vaccination, etc. News18 took these questions from the people and a few more to renowned pulmonologist and AIIMS Delhi director Dr Randeep Guleria. Here’s what he had to say:
We understand that the virus has mutated, it mutates to survive. Are there new symptoms that you’re seeing in patients that were not seen in the first wave?
By and large, the symptoms are the same: fever, cold, body aches, pain in the throat. In a relative number, we are seeing more people who may have gastric symptoms in the form of pain in the stomach, diarrhoea, loose motion, nausea, vomiting, with or without fever. So I keep telling all my patients who present with a stomach upset without even respiratory symptoms that, in the time of the Covid primarily, they should also get themselves tested.
Is the Indian variant more deadly, or is it a lack of hospital beds, and oxygen and medicines that is killing people?
So I don’t think we have enough data, although there is data being accumulated to see whether the new variants are more virulent. Whenever we have a new variant, we try to collect data to look at three or four things. The first thing that you want to look at is, is the new variant more infectious? We know that the virus wants to spread more. And variants do evolve to become more infectious to spread more rapidly and infect more and more people. The second thing we want to understand is, is the new variant more virulent? Is it causing more death? And the third is, does it have any immune-escape mechanism? Has the variant developed an immune-escape mechanism so that it causes reinfection…or the efficacy of the vaccine coming down? Currently, as far as variants in India is concerned, we could say that based on whatever limited data that we have, it does seem the virus has become more infectious. And that is why we’re seeing this huge spike in the number of cases in such a short period of time. As far as mortality is concerned, our mortality still continues to be low, but it’s still more than what we would like it to be. And that is related to both the factors that you said. One is of course related to the fact that we are not sure whether this variant is causing more mortality, but also because the healthcare structure is getting strained, there is more pressure on the healthcare structure, there can be certain areas decreasing in the quality of care, which may also indirectly be contributing to the mortality.
Many people have got Covid in the second wave. And they are saying we did not step out anywhere, we were very careful, we have got vaccinated, then how can we get Covid?
It’s very important to understand how it’s an airborne or droplet infection. And, therefore, you may not have stepped out…I know people who said my parents never went out of the house, but they got the repair person to come in to clean the AC…because of the summer coming the AC had to be cleaned, or the maid came in and had to clean up the room or do the cooking. So you may not have gone out but the person who is asymptomatic but infectious may have come into your house and spread the infection in the home environment. Therefore, saying that you did not go out may not be enough. You have to be careful about what is or who is coming into the house. And understand, many people are infectious, have Covid-19, but are asymptomatic or pre-symptomatic. So they are still infectious. So if you have a person who says I have no symptoms, that is not a guarantee that he doesn’t have Covid-19. And I keep saying this to all individuals that when you go out, when you meet people, assume everyone is positive unless proven otherwise. And take all the precautions that you would take if a person was positive. When you meet anyone, wearing your mask, maintaining your physical distancing, washing your hands should be done for everyone who you meet inside or outside the house because you don’t know who is positive.
Has it been established beyond doubt that Covid-19 is airborne? We know a Lancet study is saying so. And in that case, do protocols change?
I don’t think that protocols will change to a large extent. I’ll try to explain this to you. This is a debate which has been going on for more than six months, whether it is droplet or aerosol, and in my mind, it is a mixture of both. What is the difference between the two? Droplet infection means that the size of the particle is larger. And, therefore, because the droplets carrying the virus are of larger size, the virus cannot travel for a longer distance and cannot stay in the air for a long time and quickly drops on surfaces and the surfaces get infected. So that is why in the initial part, we were focusing a lot on surface cleaning also as a part of droplet infection. But a lot of people have been showing data for the last, I would say, seven to eight months, that along with droplet, there is also aerosol transmission. Aerosol means that this virus also can get transmitted when someone coughs or sneezes, with smaller particles, which are smaller in size, less than five microns. And they are the ones which can stay in the air for a longer period of time, can travel for a longer distance and don’t drop down to the surfaces. So you may have a person in an indoor environment who is more than two metres away from you, is coughing, and viruses stay in the environment, in the air, for a longer period. And if you cross that area, you may have a chance of getting the infection although you were always away from him by two metres. And that is why wearing your mask properly and even double masking at times is more important. And having good cross ventilation in an indoor environment is very, very important. So open your windows, make sure that if there is fresh air coming in and you are having a situation where there’s any, let’s say, airborne infection therein, the indoor air is blown out and fresh air comes in.
What are the types of masks that you recommend should be used now?
It depends on what is available. I’ll start with what is an ideal situation, literally, in a doctor’s office or in a hospital will have…this is an N95 mask. So if you can wear an N95 mask, that will be helpful. But then an N95 mask may not be easily available. Then what one can do is use a double mask, where the inner part is what we call a triple-layer surgical mask. And on top of that, you can have a cloth mask. If that is also not available, then two layers of cloth masks can also be done. But the best efficacy that has been shown in various studies is with N95 masks, which is more than 90%. 85 to 90% is if you were to use a surgical mask and on top of that a cloth mask when you’re going out, and below that is wearing a cloth mask. But having said that, I think not only wearing a mask is important; wearing it properly is also important. So whenever you use a mask, make sure that it tightly fits around your nose and mouth so that air does not come in from the side of your nose or from the side of the cheek. Because remember, you have to have air coming in from the filtering mechanism of the mask so that the virus cannot go into your nose and mouth. If the air comes in from the side without the filter, you will get the infection. Therefore, whenever you use the mask, make sure that you press it properly around your nose, around your cheeks. And you see that the chin is also properly covered so that air is coming in from the mouth. You could even take a deep breath and if the mask comes in that means air is being sucked in through the mask and you can be a little bit reassured that the mask is working properly. So these are the double-layered masks and the precautions that you need to take while wearing them. Also, when you wear a mask, before wearing a mask, wash your hands properly. When you take your mask off after you come out, again, wash your hands properly so that you don’t get the infection on your hand if the mask is contaminated.
Given the situation at hospitals right now, given how quickly the infection is spreading, the virus is spreading, should a person go for a second dose of the vaccine and expose themselves? Is it worth the risk?
First of all, you should definitely go for the second dose because the first dose will not give you that much protection as the second dose will. And we know now from a lot of data that is emerging that there is still a significant chance of infection even if you’ve just taken one dose and therefore if you can take both the doses, it is better. Secondly, most vaccination sites are not inside the ward or the Covid area of the hospital. They are at a different site. So the chances of getting infection there is very, very low. It is the same as if you stepped out and went, let’s say, to the market. So therefore I don’t think that the risk is higher if you go to a Covid vaccination site, and many vaccination sites are situated way out of the hospital setting. So it’s quite safe. But having said that, Covid-appropriate behaviour is still important when you go out for either vaccination or for any other activity.
If I have been exposed to a Covid-positive patient, when should I get tested? And what should I do if I have no symptoms? Because testing is becoming virtually impossible, if not very, very difficult right now.
So two things. One is if you have had close contact with a Covid-positive patient, and close contact means that you have spent more than 15 minutes with someone at a distance of less than two metres, and both of you…one of you, was not wearing a mask, then you are in close contact. But if you have had a close contact with a family member and you are not wearing a mask, then the first thing to do is to quarantine yourself. You must move into a separate room so that if you are infected, you do not infect others. There is no point getting yourself tested on the same day because all infections have what we call an incubation period. That is the time between getting the infection and developing symptoms or having enough viral load in the nose and throat for the test to be positive. You may get, otherwise, a test which will be negative, but will be negative because you don’t have enough virus in your throat to be picked up by the test. So normally, we advise our patients to wait for five to seven days. And after five to seven days get the test done. And if the test is negative, you are asymptomatic, then the chances of getting the infection is very, very low.
If I have mild Covid, am I safe enough to mingle with people after 14 days? Do I need to get a test after 14 days?
If you have mild Covid and you have been asymptomatic after the tenth day, or you have had no fever for at least three days before this, and you have currently no symptoms in your last 14 days, then you are totally non-infectious. You need not worry. You can mingle with people and you don’t need to get the test done.
The first wave seemed to have spared the young children, but not the second wave. In Brazil, there are deaths being reported in babies and young children. In Mumbai, there’s a 65% jump in Covid-positive paediatric cases. Why is this happening? And what can parents do?
I think, again, the reason for this happening needs to be evaluated. But the most obvious reason seems to be the fact that when we had the first wave, we really protected the children, we were very careful to see that they did not go out, schools are all closed. And we really made sure that they did not get infected. Currently, what has happened is that schools opened up, children were going out. There were holidays planned where the children went out for holidays. And that’s a susceptible population, which was really not infected and had no immunity, suddenly got exposed to a virus, which is very infectious. And that’s why it’s spread rapidly in the younger age group. Also, the viruses change and like you asked me in the beginning, we need to really find out whether now it has evolved to cause more severe illness even in the younger age group. Current data needs to be looked at more critically in terms of the severity of illness and mortality in children as compared to the older age group. I think still the mortality is higher in the older age group as compared to children. But we need to be very vigilant and develop treatment protocols so that we have effective treatment strategy for the younger age group
Given that the kids, even if they get infected, are lacking full-blown symptoms, are they then silent carriers of the infection?
So children are known to have very mild illness or have any minimal problem and that is why there was a whole concern that once schools open and children get infection, they may not have that many symptoms, but they could carry the infection to their houses and there the elderly, the grandparents or parents, who get infected or people with comorbidities would get infected, and this would lead to higher mortality. So the children need to be protected not only from the point of view of them getting infected, but from the point of view of them carrying the infection to the grandparents who are most susceptible and can get severe infection.
Read all the Latest News, Breaking News and Coronavirus News here. Follow us on Facebook, Twitter and Telegram.

















Comments
0 comment