
views
Tapering off Your Meds Slowly

Don’t go “cold turkey” to quit your medication. Despite the uncertainty surrounding the causes of brain zaps, it’s well accepted that abruptly quitting certain medications is a common trigger. SSRI and SSNRI antidepressants are most commonly associated with brain zaps, so it’s important not to quit your antidepressant all at once. Quitting an antidepressant “cold turkey” can also lead to other severe physical and emotional withdrawal symptoms. Do not quit an antidepressant without your doctor’s guidance. The process of quitting other medications is also sometimes associated with brain zaps, including benzodiazepines (for anxiety or muscle relaxation) and the ADHD medication Adderall. Quitting use of the illicit drug MDMA (ecstasy) may also trigger brain zaps. As with antidepressants, quit under your doctor's guidance. It's especially important to work with your doctor and taper off benzodiazepines. Stopping these medications suddenly can be dangerous and may even cause seizures if you've been taking them daily.
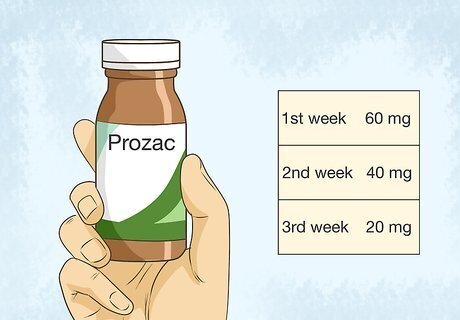
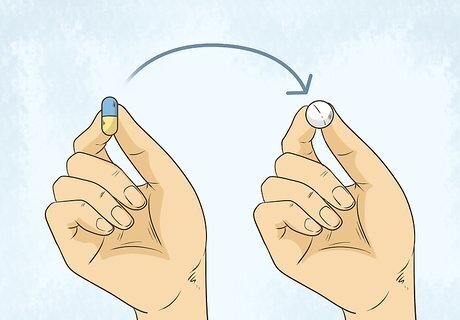
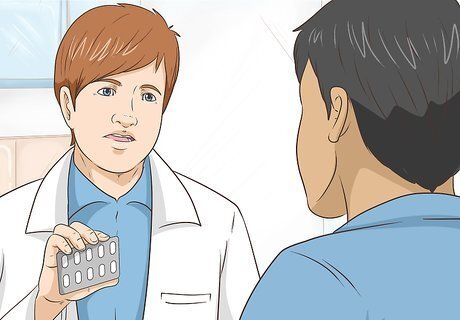
Follow your doctor’s tapering instructions carefully. Instead of quitting your medication all of a sudden, you should slowly reduce your dosage over a period of several weeks to several months. The slower you go, the less likely you are to experience brain zaps, although some people get them regardless of how slow they taper. For instance, you might reduce your daily dose of Prozac in 1-3 week increments along the following schedule: 60 mg; 40 mg; 30 mg; 20 mg; 10 mg (actually 20 mg every other day). Some doctors even recommend what is known as titrating off of an antidepressant, which involves opening each capsule and removing an increasing amount of the “beads” inside. Do not attempt this without your doctor’s guidance, however.

Make sure you don’t miss doses while tapering (or any other time). Some people experience brain zaps almost as an “alarm clock” that alerts them to a missed dose of medication. To avoid this, set less uncomfortable reminders to take your medication on a consistent schedule. Set a reminder on your phone, for example, so you take your meds at the same time each day. While tapering, you'll typically just reduce the dose of the pill you take, not change the timing or frequency for taking it. Clarify with your doctor what you should do if you miss a dose. Don’t try to catch up or double up on a dose unless specifically instructed to do so by your doctor.
Transition to second "bridge" medication if you need help tapering off the first. It’s possible that the period of time an antidepressant remains active in your body (sometimes called its “half life”) will impact your withdrawal symptoms, including brain zaps. Temporarily transitioning to a "bridge" medication with a longer “half life,” such as Prozac, may help reduce or eliminate your brain zaps. For instance, if you’re tapering off Cymbalta, your doctor may prescribe increasing doses of Prozac as you taper down your Cymbalta doses. Then, once you’re off Cymbalta, you’ll taper off the Prozac. Do not attempt this without your doctor’s guidance.

Go back on your meds only if your withdrawal is debilitating. With patience, perseverance, and support, most people can stick it out past the brain zaps and other withdrawal symptoms. If your symptoms are intolerable, however, your only option may be to go back on the medication temporarily and try tapering off again at another time. Talk to your doctor about the pros and cons of resuming a medication that you’re trying to taper off of. There's no established timeline for how long you should wait between attempts to taper off a medication. Work with your doctor to determine the best timing for you. You may not necessarily experience the exact same withdrawal symptoms the next time around. Withdrawal symptoms can change due to unknown factors, or because you're tapering in a different fashion (such as tapering more slowly).
Making Behavioral Adjustments
Use calming activities to reduce your stress levels. Getting off antidepressants is stressful, and dealing with brain zaps only makes it worse. Some people report that their brain zaps are more frequent and/or severe when their stress level is elevated, so try different calming activities to help alleviate your stress. Activities like yoga, deep breathing, meditation, a warm bath, or listening to soothing music may help. Light exercise (such as walking or easy biking) may be calming for you, but, in some cases, it can also bring on brain zaps. Some brain zap sufferers believe that the calming effects of aromatherapy are particularly helpful. For example, putting drops of lavender, bergamot, or rose in a diffuser may prove beneficial.

Avoid making lateral eye movements or similar triggers. Moving your eyes side to side rapidly is a common trigger for a brain zap. Some people report that moving their entire head side to side or up and down has the same effect. If you identify a similar trigger in your case, work to avoid that activity. For instance, if lateral eye movement is a trigger for you, don’t try to follow the ball while your friends play table tennis.

Remind yourself that the zaps aren’t harmful and will eventually stop. Brain zaps are real, frustrating, disorienting, and sometimes even painful. However, there is no evidence that they cause any type of short- or long-term damage. Also, although it may take weeks, months, or rarely even years, they nearly always stop eventually. Keep telling yourself that you can get through this, and rely on your support network—friends, family, and your medical team—for help. One theory for brain zaps is that they are related to a drop in a “calming chemical” in the brain known as GABA. Quitting an antidepressant or certain other drugs (such as benzodiazepines and Adderall) can cause a temporary drop in GABA levels. Over a period of weeks to months, your GABA levels should return to normal.
Trying Unproven Remedies

Increase the amount of water you drink. If, as some experts believe, brain zaps are related to a drop in the “calming chemical” GABA in the brain, then drinking more water shouldn’t directly help. However, like several other unproven remedies, some brain zap sufferers swear by its beneficial effects. Fortunately, drinking more water is good for practically everyone, and it’s extremely difficult to drink so much water that it becomes harmful. Staying adequately hydrated can help you feel better physically and emotionally, which might make brain zaps less noticeable.
Eat a nutrient-dense diet. Like with drinking water, there’s no direct scientific evidence that connects your diet to brain zaps. However, eating a healthy diet full of nutrient-dense foods is certainly good for your overall physical and mental wellbeing. Eat a variety of fruits and vegetables every day to get a wide range of nutrients. Complement this with whole grains, lean proteins, and healthy fats. Cut back on nutrient-poor foods like sugary drinks and packaged snacks.
Talk to your doctor about taking Benadryl to reduce brain zaps. Benadryl is the most common brand name for the antihistamine diphenhydramine, and some brain zap sufferers claim that it provides relief. It’s not clear why Benadryl would help, but it may be worth discussing the option with your doctor. Benadryl and other forms of diphenhydramine can be purchased over the counter, but you should still talk to your doctor before trying it. Benadryl can interact with other drugs and cause significant side effects in some cases.
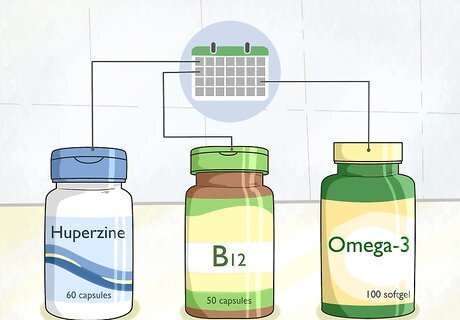
Give various supplements a try if your doctor agrees. There’s no evidence that any particular supplement will offer relief for brain zaps. Your best option may be to try one contender for several days to a week, then move on to another if your brain zap symptoms don’t improve. Some of the most commonly mentioned supplements for brain zaps include omega-3, B12, spirulina, and huperzine. Talk to your doctor before trying any new supplement, due to the risk of drug interactions or side effects.














Comments
0 comment