
views
X
Research source
While your risk of developing T2D is very high and diabetes has grown to worldwide epidemic proportions, this can be reversed by losing weight, changing the way you eat, and through exercise.[2]
X
Trustworthy Source
National Institute of Diabetes and Digestive and Kidney Diseases
Health information from the National Institute of Diabetes and Digestive and Kidney Diseases, a division of the U.S. National Institutes of Health
Go to source
[3]
X
Research source
[4]
X
Research source
Polonsky, KS., The Past 200 Years in Diabetes. New England J of Medicine, (2012) 367:1332-1340.
Controlling Insulin Resistance Through Diet

Pick complex carbohydrates. Try to make most of your carbohydrate intake consist of complex carbohydrates. This means that they're more complicated molecularly and take longer for your body to break down. This may help your body break down glucose and may help you feel fuller longer, controlling weight and appetite control. Examples of complex carbohydrates include whole unprocessed foods like: Whole grains Peas Lentils Beans Vegetables

Avoid processed foods. Try to keep your food as close to its original or natural form. To do this, limit processed or prepared foods and cook from scratch as much as possible. Processed food often contains large amounts of sugar. Read labels to determine how much sugar is in a product, but realize that manufacturers are not required to list added sugars. An easy way to avoid processed foods is to avoid "white" foods (no white bread, white pasta, or white rice). For example, one 6-ounce serving of flavored low-fat yogurt has 38 grams of sugar (which is the equivalent of 7 teaspoons of sugar).

Cut back on sugary drinks and simple carbohydrates. While sugars alone don't cause diabetes, eating more high-fructose corn syrup is linked to an increased risk of insulin resistance, T2D, cardiovascular disease, and obesity. Avoid simple carbohydrates that contain glucose, sucrose, and fructose. These include: Soft drinks Sweeteners: maple syrup, honey, table sugars, jams Candies, cakes, pastries
Increase your fiber intake. Studies have shown that eating insoluble fiber along with whole grains can reduce your risk of T2D. Try to eat insoluble fiber with each meal. For example, you can sprinkle one tablespoon of ground flaxseeds over each meal. Good sources of fiber include: Brans: corn bran, oat bran, wheat bran Beans: navy beans, lentils, kidney beans Berries: elderberries, raspberries, blackberries Whole grains: bulgur, brown rice, barley, oats Vegetables: peas, leafy greens, squash Seeds and nuts Fruits: pears, prunes, dried figs

Eat more lean meat and fish. Lean meats and fish are good low-calorie sources of protein. Make sure any meat you choose is not only lean, but skinless (since the skin is high in animal fat, added hormones, and antibiotics). Look for wild-caught fish such as salmon, cod, haddock and tuna. These fish are good sources of omega-3 fatty acids that are essential for your health and are anti-inflammatory. Try to eat at least 2 servings of fish each week. Limit red meats like pork, beef or lamb. These have been linked to T2D, cardiovascular disease, and colorectal cancer.

Include more fruits, vegetables, and herbs. You don't need to avoid fruit for fear that it contains sugar. The sugars in fruit are combined with the fiber which slows the absorption of sugars. Try to get 5 servings of fruits and vegetables every day. Don't forget to add herbs that can control your blood sugar levels. These can also help you fight sugar cravings and are safe with no side effects (when taken in commonly used amounts as food). Use these herbs: Cinnamon Fenugreek Okra (not quite an herb, but more of a side-dish) Ginger Garlic and onions Basil Bitter melon (more commonly used as a tea three to four times a day)
Increasing Your Activity Level

Exercise for 30 minutes a day. Moderately increasing your physical activity can help reverse insulin resistance. You don’t have to get ready for a marathon. Just choose a physical activity that you enjoy or are interested in picking up. This way, you're more likely to become active. You may start walking more, climbing more stairs, doing more outdoor activities, hiking, gardening, aerobics, Tai chi, yoga, using an elliptical, using a rowing machine, using a stationary bicycle, or stretching. Consider whether you want to work out alone, with someone else, or play a group sport.

Start slowly. Start with 10 minutes of activity a day. When you're comfortable with that level of activity, add a few minutes every week. For example, you may tell yourself to walk more. You might try parking your car farther from the office or getting off of the elevator two or three floors early so you can take the stairs the rest of the way. Increase these amounts by parking even farther away or taking more flights of stairs. Avoid setting an extreme goal for yourself early on. You'll be more likely to remain active if you set small, achievable goals.

Become comfortable with more physical activity. Once you've been working out for a while, start to challenge yourself. Work yourself up to 30 minutes of activity a day for at least 5 days of the week. To keep things interesting, you may want to mix up the activities you do. For example, you might swim for 20 minutes and jog for 10 minutes one day. Consider joining a gym and getting a personal trainer. This way, you'll understand how physical conditions can impact your physical activity. A trainer can help you design a personalized fitness plan.
Diagnosing Insulin Resistance
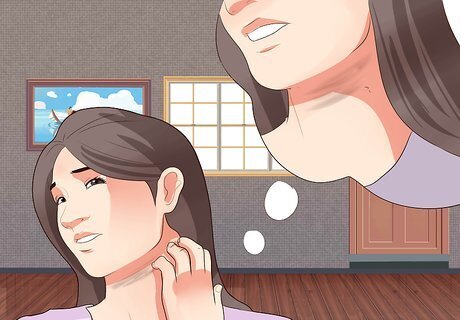
Watch for insulin resistance symptoms. If you notice the skin around your neck, armpits, elbows, knees, and knuckles get darker, you may have a skin condition known as acanthosis nigricans. This is an early sign that you're at risk for T2D and insulin resistance. You may also have increased hunger, thirst, fatigue, weight gain, or increased urination.

Consider your risk. There are many things that increase your risk of insulin resistance. These include: Being overweight or obese Being physically inactive or sedentary High blood pressure Low HDL cholesterol (“good cholesterol”) levels (less than 35 mg/dL) High triglyceride levels (over 250 mg/dL) Being older than 45 years old Having a family history of diabetes Having a history of gestational diabetes, giving birth to a baby with a birth weight of more than 9 pounds or a history of polycystic ovary syndrome (PCOS) For women, having a waist measurement of more than 35 inches For men, having a waist measurement of more than 40 inches

Get a diagnosis. Often, insulin resistance has no symptoms. Instead, your doctor may notice your blood sugar is higher than normal. The doctor then will run one of these tests: A1c: This test measures how your body has handled sugars for the last 3 months. An A1c result of over 6.5% is a diagnosis for T2D while insulin resistance is diagnosed at levels between 5.7 and 6.4%. Fasting blood glucose test: You'll need to fast for several hours. Then, your blood is drawn to measure blood sugar levels. Fasting blood sugar levels between 100–125 mg/dL suggest insulin resistance. Oral glucose tolerance test (OGTT): Your blood is drawn to measure blood sugar levels. You'll then drink a very sweet beverage and have your blood drawn two hours later. Your blood sugar is measured again. This test determines how well your body handles sugars.

Talk with your doctor. Once you've been diagnosed with insulin resistance, you should get regular checkups. Talk with your doctor about any dietary changes you've made, weight loss plans, and your activity levels. Your doctor will want to do regular blood tests to check your blood sugar levels. Track your labs and use them as motivation to keep making diet and lifestyle changes.

Talk to your doctor about medication. Once you have been diagnosed as prediabetic, you may want to take a medication that helps control your blood sugar, such as metformin. Ask your doctor about using this in combination with lifestyle and dietary changes to delay or reverse the onset of type 2 diabetes.


















Comments
0 comment