
views
Identifying a Herniated Disk

Recognize the symptoms. The most frequent areas for herniated disks are in the lower spine and the neck. If your herniated disk is in your lower back, then you will probably have pain in your legs. If the herniated disk is in your neck, then your shoulder and arm will probably hurt. Symptoms include: Pain in your limbs. The pain may become more intense when you cough, sneeze, or move in certain ways. Numbness or feelings of pins and needles. This occurs when the nerves that run to that extremity are affected by the herniated disk. Weakness. If your lower back is affected you may be more likely to trip and fall. If your neck is affected, you may have difficulty carrying heavy items.

Go to the doctor if you think you have a herniated disk. The doctor will do a medical exam to determine exactly where your pain comes from. The doctor will likely ask about your medical history including any recent injuries. The doctor may also test your: Reflexes Muscle strength Coordination, balance, and ability to walk Sense of touch. The doctor may test whether you feel light touches or vibrations on various different areas of your body. Ability to raise your leg or move your head. These movements stretch the spinal nerves. If you get increased pain, numbness, or pins and needles, it may suggest that a disk is herniated.

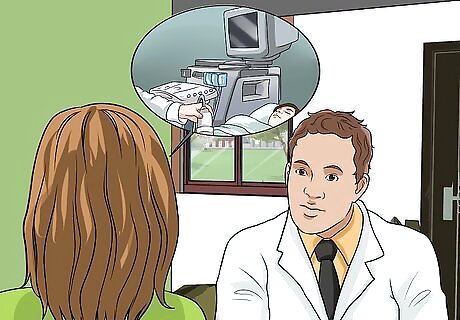
Get imaging tests if your doctor recommends it. These tests can be used to exclude other possible causes of your pain and to let the doctor see exactly what is happening to your disks. Tell your doctor if you are pregnant or think you could be pregnant because it may influence which tests the doctor recommends. An X-ray. Your doctor may ask you to get an X-ray to verify that your pain is not caused by an infection, tumor, broken bone, or misalignment of the bones in your spine. The doctor may also suggest a myelogram with the X-ray. This involves putting dye into your spinal fluid which will show up on an X-ray. It helps the doctor see where disks might be pressing on your nerves. A computerized tomography scan (CT scan). During a CT scan you will lie on a table that moves into the scanner. The scanner will take sequential X-rays of the area of interest. The doctor may ask you to hold your breath briefly to make sure the picture will be clear. It will not hurt, but you may be asked to fast for a few hours before the test or be given a contrast dye beforehand. The test will probably take about 20 minutes or less. This test can help the doctor determine exactly which disks are affected. Magnetic resonance imaging (MRI). An MRI scanner uses magnets and radio waves to create pictures of your body. An MRI is especially useful for determining exactly which disk has herniated and what nerves it might be pressing on. This test does not hurt, but requires that you lie on a table that will slide into the scanner. The scanner will make loud noises and you will probably get earphones or earplugs to wear. It may take up to an hour and a half. This is the most sensitive imaging test, but also the most expensive.

Get nerve tests. If the doctor is concerned that you may have damage to your nerves, you may be asked to get nerve conduction tests and an electromyogram. During the nerve conduction tests the doctor may administer a small electrical pulse to determine if it is correctly conveyed to specific muscles. During the electromyogram, the doctor inserts a thin needle into your muscle to measure the electrical pulses that arrive. Both procedures may be uncomfortable.
Using Home Remedies and Lifestyle Changes

Apply ice or heat as needed. The Mayo Clinic recommends these as home remedies for dealing with the pain of a herniated disk. Which one you chose to use may depend on the stage of your injury. In the first few days, cold packs can help reduce inflammation and swelling. You can use an ice pack or package of frozen vegetables wrapped in a towel. Apply it for about 10 minutes, then give your skin a chance to warm up. Do not apply the cold pack directly to your skin. After the first few days, you can use warmth to relax tense muscles. Use a hot water bottle wrapped in a towel or a heating pad. Do not put the heat source directly on your bare skin to avoid burns.

Stay active, if you can. You may need to rest for the first few days after the disk herniated, but after that, staying active will keep you from stiffening up and help you recover faster. Talk to your doctor or a physical therapist to find out what exercises they may recommend for you. Avoid doing activities that could make it worse. This may include carrying heavy items, lifting, or reaching. Your doctor may suggest swimming because the water will support your weight and relieve the pressure on your spine. Other possibilities include biking or walking. Try pelvic tilts if your doctor approves it. Lie on your back with your knees up and put your hand beneath your lower back. Tilt your pelvis so that you are pushing down on your hand. Hold it for five seconds. Repeat this 10 times. If this causes pain, stop and talk to your doctor. Do buttock squeezes. While lying on your back with your knees up, squeeze your buttocks together and hold it for five seconds. Repeat this 10 times. This should not cause pain. If it does, do not continue and discuss it with your doctor.
Adjust your sleeping position. You may get relief by lying in positions that take the pressure off your spine and your nerves. Your doctor or physical therapist may suggest: Lying on your stomach on pillows so that your back is rounded. This may reduce the pressure on your nerves. Lying in the fetal position with a pillow between your knees. The side with the herniated disk should be up. Lying on your back and stacking pillows underneath your knees so that your hips and knees are bent and your lower legs are parallel to the bed. During the day you may want to lie on the floor and rest your legs on a chair.

Get social support. Living with chronic pain is extremely stressful and can trigger depression and anxiety. Maintaining your social network will help you to cope and feel less alone. You can get social support by: Talking with friends and family. If there are physical activities that you can no longer do alone, let them help you. See a counselor. A counselor can help you learn coping techniques and determine if you have unrealistic expectations for your recovery. Your doctor may be able to recommend someone that specializes in helping people cope with pain. Join a support group. This may help you to feel less alone and to learn coping mechanisms.

Manage stress. Stress makes you more sensitive to pain. By developing techniques for dealing with stress, you may be able to better handle the pain. Some people benefit from the following techniques: Meditation Deep breathing Music or art therapy Visualizing calming images Progressive tensing and relaxing the different muscle groups in your body
Talk to a physical therapist about alternative therapies. There may be ways that you can change how you move or sit to avoid making your condition worse. You may also benefit from alternative methods of pain management, but always talk to your doctor to be sure that these methods will be safe for you. Possibilities include: Short-term bracing for your neck or back to protect it and give you stability Traction Ultrasound treatments Electrical stimulation
Taking Medications
Deal with moderate pain with over-the-counter painkillers. This is likely to be the doctor's first suggestion if your pain isn't too severe. Possible medications include ibuprofen (Advil, Motrin IB) or naproxen (Aleve). Though non-steroidal anti-inflammatory drugs (NSAIDs) can be very helpful, they may not be right for you if you have high blood pressure, asthma, heart or kidney problems. Talk to your doctor about these medications before you start because they can interfere with other medications, including herbal remedies or dietary supplements. NSAIDS are especially known to cause gastric ulcers. Consult your doctor if over-the-counter medications do not help within 7 days.
Combat severe pain with prescription medications. Depending upon your symptoms and medical history, your doctor may suggest: Nerve pain medications. These medications are increasing in their popularity because the side effects are often less severe than those produced by narcotics. Common ones include gabapentin (Neurotin, Gralise, Horizant), pregabalin (Lyrica), duloxetine (Cymbalta), and tramadol (Ultram). Narcotics. These medications are likely to be prescribed when over-the-counter medications weren’t strong enough and nerve pain medications weren’t helpful. They may cause side effects including sedation, nausea, confusion, and constipation. These medications often have codeine or a mixture of oxycodone and acetaminophen (Percocet, Oxycontin). Muscle relaxants. Some people get painful muscle spasms and these medications can help this. A common one is diazepam. Some muscle relaxants may cause sedation and dizziness, so they are best used at night, just before bed. Read the packaging to determine whether you should avoid driving or operating machinery while taking them.

Get cortisone injections for the pain. Cortisone can suppress inflammation and swelling. If need be, your doctor may offer to give you an injection directly into the area that is causing the pain. Your doctor may also use oral steroids when trying to decrease swelling. Corticosteroids are often used to delay or possibly eliminate the need for surgery.The hope is that once the inflammation goes down, the body will naturally heal over the long-term. When given at high doses over the long-term, cortisone can cause weight gain, depression, diabetes, high blood pressure, osteoporosis, increased bruising, acne, and a vulnerability to infections.
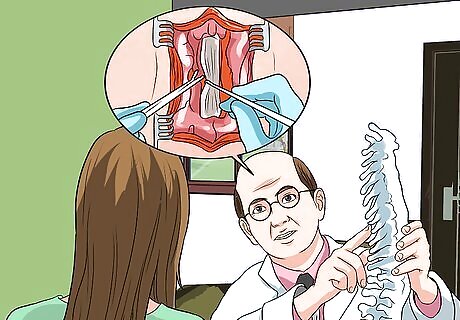
Discuss surgery with your doctor. Your doctor may recommend surgery if other options are not improving your symptoms, your nerves are badly compressed. There a few different types of surgery your doctor may suggest: Open discectomy. During this procedure the surgeon makes a cut into your spine and takes out the damaged part of the disk. If the damage is extensive, the surgeon may remove the whole disk. If the whole disk is removed, it may be necessary to fix the vertebrae around the missing disk to give you stability. This is called fusion. Prosthetic intervertebral disk replacement. During this procedure, after the surgeon removes the damaged disk, it is replaced with a prosthetic disk. Endoscopic laser discectomy. During this procedure the surgeon will make a small cut into your spine, then insert a thin tube that has a light and a camera on it (an endoscope). The damaged disc will then be removed using a laser.

Follow your doctor’s instructions when recovering from surgery. Surgery helps most people who get it, but it may take you several weeks to recover. You may be able to go back to work after two weeks to a month and a half after the surgery. If you notice signs of any complications arising from the surgery, contact your doctor immediately. Though rare, possible complications include infections, damage to the nerves, paralysis, hemorrhaging, or temporarily losing sensitivity to touch. Spinal surgery works for a while. But if the patient fuses two vertebrae, the load is often transferred to the next adjacent vertebrae, which may require additional surgery. An important question to ask the doctor is if you may require additional surgeries in the future.


















Comments
0 comment