
views
X
Trustworthy Source
National Health Service (UK)
Public healthcare system of the UK
Go to source
A stroke can be frightening for both the person who experiences it and the friends and family around them who will have to adapt to a new situation. When a loved one has a stroke, you will likely need to make adjustments to assist them in their recovery, and these changes may be temporary or permanent. Experts note that it is important to always remember that your loved one will likely have some natural healing over time and can improve even further with therapy.[2]
X
Research source
While you are helping your loved one recover from a stroke, it is essential to take care of yourself as well.
Helping Your Loved One Overcome Difficulties
Make your home easily accessible. While each person will experience different effects from a stroke, hemiparesis (or weakness) of the whole side or just the arm or leg is a common result of a stroke. In addition, problems with balance and coordination are common, too. Thus, adjustments may need to be made to ensure that your loved one (who may now have mobility difficulties) can easily access her house. When attempting to make your house stroke-survivor-friendly, consider the following suggestions: Move the person’s bed to the ground floor so that she can avoid having to use the stairs, where falls are more likely to occur. Clear a path to all essential rooms (including bedroom, bathroom, and kitchen). Less clutter will mean that your loved one is less likely to fall. This includes removing area rugs. Install a seat in the shower to allow her to sit while bathing. Additionally, install handrails to assist with getting in and out of the tub and/or shower as well as by toilet to help her get up and down if needed. Make a bedpan readily available at her bedside. Encourage use of this commode, especially if the person feels off-balance or disoriented as this can avoid falls which could further injure the patient. If stairs cannot be avoided, install handrails around the stairs to assist your loved one move up and down. The person's physical therapist should be working with the person to re-learn how to navigate her environment, including going up and down stairs.

Assist with mobility. A new deficiency in mobility is one of the most common issues faced by stroke survivors. A person who was once very mobile and independent may be reduced to slow, unsteady walking or even be largely bed-bound after a stroke. Expect your loved one to require some assistance moving around for at least a period of time after a stroke. Assistive devices can be used to better facilitate mobility. Family members can consult a physical therapist in order to find out which assistive devices would best suit the stroke survivor. These devices could include a wheelchair, walker, or cane depending on the severity of mobility issues. Support and encourage your loved one in his attempts to be mobile. Celebrate any reduction in dependence on assistive devices.

Create a secure environment. Falls and accidents after a stroke are, unfortunately, very common. Make your loved one’s safety a priority to avoid any unnecessary side effects or complications that are related to, but not a direct result of, her stroke. Put up rails around the stroke survivor’s bed and lower the level of the bed as necessary. The rails should be up at night to prevent any falls due to imbalance or disorientation, and the bed can be lowered to avoid the need to “climb” into bed. If something that is frequently used (for example, pots and pans) are located somewhere that is hard to access (like in a high cabinet), move them. Make commonly used items in locations that are easy for your loved one to access. Be present to assist with tree trimming, snow shoveling, house painting, or any other activities that put your loved one at an increased risk for an accident after her stroke.

Learn feeding and eating techniques. Dysphagia is the medical term that means a person is experiencing difficulty swallowing. After a stroke, eating or drinking can become difficult because the muscles of chewing and swallowing can be weakened (this is particularly true immediately after a stroke). Thus, it is important to help your loved one adapt to new habits of eating and drinking to ensure he is getting adequate nutrition. After a stroke, it is common to have a nasogastric feeding tube in the early stages; however, in especially severe cases, a feeding tube will be a permanent requirement in order for the stroke survivor to receive the necessary nutrients. If the stroke survivor is feeding through percutaneous endoscopic gastrostomy (PEG) tube — a tube used for feeding that is inserted directly in the stomach- make sure that the tube is intact, functioning properly, and protected from infection and from pulling by the patient. Your loved one will need to undergo a test called a swallowing study, which will allow his doctor to assess his ability to swallow food. Speech therapy and x-rays are used to help the doctor determine when it is safe for the patient to move from liquids to thick, soft foods. When your loved one is able to eat without assistance of a medical device, feed him thick, soft food. Stroke survivors who are starting to feed orally must start with this type of food to prevent aspiration pneumonia. There are liquid thickeners in the market that can help make soup and juice thicker. You can also use items in your kitchen like gelatin, cornmeal, and oats. Keep your loved one upright while eating in order to prevent aspiration pneumonia, which occurs when food is inhaled into the lungs. Because his muscles involved with swallowing are weak, his position for eating is even more important. This will ensure mealtimes are safe and remain a fun part of the day.

Identify issues with incontinence. A stroke may change the control your loved one has over her bladder and bowels. This can create safety problems (for example, infections or sores) and can also be a sore subject or one that causes great embarrassment. As a caretaker, it is important to recognize if these issues are occurring and address them with your loved one in order to help her on the road to recovery. For stroke survivors that are unable to use a commode or go to the bathroom, adult diapers may be used. These can be found in almost any drug store or grocery store. Encourage your loved one to wear one if necessary until she regains control of her bodily functions. You will need to assist your loved one by making sure the diaper is changed immediately after each time she voids or has a bowel movement. Otherwise she may experience skin breakdown and sores and potential infection in the area.

Address communication issues. Most stroke survivors have certain levels of communication impairment, at least temporarily. The severity of the stroke may determine how severe the communication impairment is. Some stroke patients might not be able to express themselves correctly, while others might not be able to understand what is being said. Due to paralysis, some stroke survivors might not be able to say words properly, though the cognitive aspect of their communication is functioning. It is important to help your loved one deal with communication issues. Before considering speech impairment, make sure that the stroke survivor does not have any hearing difficulty. This can also be a cause of communication difficulty and often can be corrected with the use of a hearing aid. Learn about the different types of communication issues. For example, recognize if your loved one is suffering from aphasia (where the individual can think clearly, but has trouble getting her messages in and out) or apraxia (where the individual has difficulty putting speech sounds together in the correct way). Use short words and nonverbal communication such as hand gestures, nodding or shaking, pointing, or even showing objects. The patient should not be asked too many questions at once and should be given ample time to respond to any communication. Accept any form of communication as valid. Visual aids can be used for communication — this includes charts, alphabet boards, electronic media, objects and pictures. This can help your loved one overcome the frustration associated with not being able to communicate effectively.
Establish a routine to make your loved one feel at ease. Establishing a daily routine can make impairments such as communication less frustrating. If the stroke survivor knows the routine for the day, he anticipates the activities and the family anticipates his needs. This can relieve stress for both the patient and those caring for him.
Watch for emotional changes. Strokes can have emotional as well as physical effects. First, strokes can result in personality changes that can negatively affect relationships. Second, strokes can result in post-stroke mood disorders, including depression, anxiety, and pseudo-bulbar affect (PBA). As a caregiver, it is important to be vigilant and take notice of any emotional changes in your loved one. Depression strikes between one- and two-thirds of stroke survivors, while PBA affects approximately one-quarter to one-half of survivors. Get treatment for your loved one if necessary. Medication and counseling have benefitted many stroke survivors and is often covered by insurance.
Helping Your Loved One through Therapy
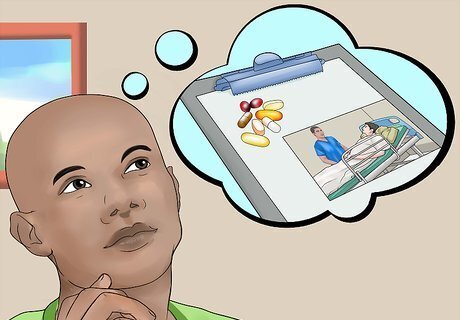
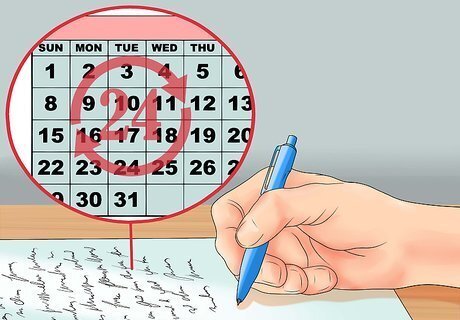
Memorize your loved one’s medication and therapy program. After your loved one is released from the hospital, it will be up to you to know the medications and therapies needed by the stroke survivor. This is an important role, and one that should not be taken lightly. It will greatly benefit your loved one’s health if you help her maintain a schedule for medicine and therapy. List all medications and times when the patient will take them. Make sure your loved one does not run out of any necessary medicine. Planning ahead is very important to avoid delays in therapy. Understand the side effects of any medications prescribed to your loved one. Be on the lookout for any of these side effects. Discuss the administration of your loved one’s medicines with her doctor. Recognize if the medicine should be administered orally or if it should be crushed in food. Know if it should be taken with food or on an empty stomach. Adherence to doctor’s appointments should also be followed to ensure that any problems that may occur during rehabilitation are managed early. This will help to prevent complications of delayed treatment. You will likely need to remind your loved one of the appointment and arrange a ride for them to the clinic. Make keeping track of your loved one’s medication and therapy easy on yourself by writing notes or setting alarms on your phone. Look for apps designed to remind you when to administer medication and utilize planners and calendars that are prominently displayed. Forgive yourself if you make a mistake. If you are late giving a pill or going to a therapy session, don't beat yourself up. Feeling guilty will not benefit your loved one nor yourself.

Acquaint yourself with therapy exercises and activities. It's wise to attend at least one therapy session in order to become better acquainted with exercises and activities that the stroke survivor must practice at home. While the therapist is performing the exercise with the stroke survivor, try also doing it with him. Having the therapist present while learning the exercises is helpful. The therapist can correct or help you improve how you help the stroke survivor during therapy exercises.

Know the rehabilitation goals made by the therapist and the stroke survivor. Knowing the goal of rehabilitation (that is, the expected outcome or outcomes) will help you better understand the time frame of rehabilitation and the progress that is being made. It can also help you push the patient further in performing her therapy exercises. Encourage your loved one not to quit on her therapy goals. Rehabilitation after a stroke can be very difficult, and it is important that you encourage your loved one to keep striving toward her goals. Oftentimes, gains in abilities can take up to six months to one year after a stroke. It is very important to partake in therapy routinely to continue to progress forward. Recognize any improvements and address non-improvement too. If your loved one is not improving after a long time in rehabilitation, speak with the doctor or therapist about adjusting the therapy regimen.

Know when to call the doctor. There are several situations during your loved one’s rehab where you may need to make a special trip to the doctor. Especially during rehabilitation, when your loved one is pushing his body to recover from a serious brain injury, it is important to keep a vigilant eye on his health. Do not ignore any falls. Falls are quite common during rehabilitation. The falls can cause further damage to the patient and worsen the condition. The patient should be taken to the hospital for a medical checkup in the case of a fall so that all serious medical issues can be ruled out. Remember that your loved one is at an increased risk of suffering from another stroke within a year of his first stroke. Know the warning signs of a stroke and know who to call if you see your loved one experiencing any of these warning signs, including: Face drooping Arm weakness Speech difficulty Sudden numbness in the face, arm, or leg, especially on one side of the body Sudden trouble seeing in one or both eyes Sudden trouble walking, dizziness, loss of balance Sudden, severe headache with no known cause
Showing Your Support

Be patient. Try to keep listening to what the stroke survivor is saying even if her speech is distorted or she is mumbling. Recognize that she wants to communicate, but is unable, and this is as frustrating to her as it is to you. Talk to her, even if she is unable to respond. Although communication might be frustrating at first, it is important that family members reinforce it. This often results in better rehabilitation of the stroke survivor. Your positive attitude and patience can help your stroke survivor get better faster.

Encourage your loved one. A patient recovering from a stroke may need months or years of rehabilitation. Stroke victims may be taught to relearn old things again; however, they may never get back to exactly how they were before the stroke. Stroke survivors may be depressed, in denial, or may feel helpless, overwhelmed and fearful. Because of this, families of stroke survivors play a very important role in the recuperating period. It is important to make the stroke survivor feel that he is not alone. In the immediate aftermath of his stroke, a stroke survivor may worry about his job, how he is going to take care of himself (or who will take care of him), and how he can rehabilitate quickly (and if he will ever be “normal” again). Talk to your loved one about his emotions. Ask him how he feels, and maintain a positive attitude regardless of the situation.

Involve yourself in your loved one’s progress. Families involving themselves in the rehabilitation of their loved one serve as strong and steadfast source of support. Understand the impairments that have resulted from your loved one’s stroke and discuss the potential for recovery with your loved one’s doctors. Understanding a bit about the recovery process can make you feel more empathetic and enable you to be a better source of support to your stroke survivor. Accompany your loved one to her therapy sessions. Participate as much as you can, provide smiles and verbal encouragement whenever possible. This is a great way to show your loved one that you are interested and invested in her recovery. At the same time, remember that this is her therapy and she needs to have decision making abilities and as much control as she can. Do not become the dictator of your loved one's life or treatment — ask her what she wants and give her as much autonomy as possible.

Support independence. After a stroke, the stroke survivor may feel helpless — do your best to empower him. He may be incontinent, having trouble communicating, and have difficulty walking — all things that we take for granted in our day-to-day lives. Provide help when you can (and when it is necessary), but encourage and support independence — whether it is a few steps without a walker, the willingness to answer a phone call, or an attempt to write a note. As the safety of your loved one is top priority, there are some things you must consider: Assess the stroke survivor (or ask a doctor or therapist for assistance) in order to better understand which activities he can and cannot do (or which ones he should not do). Being able to make this distinction will help you determine for which activities you can encourage independence without exposing your loved one to any unnecessary risk. Encourage the stroke survivor to practice activities learned during rehabilitation sessions. Do these activities with the stroke survivor until he can do it alone. Support the stroke survivor’s choice of rehabilitation. If the stroke survivor wants to rehab at home, as outpatient, or in the hospital, let him make this decision as independently as possible. When decision making skills are exercised by the stroke survivor, the family and the rehabilitation team has a better idea what the stroke survivor wants. There is a higher chance to encourage independence and see signs of healing in a stroke survivor if he is an agent in his own care.
Consider joining a network for survivors and caregivers. For example, the American Stroke Association has an online Support Network that you can join for free. By joining this network, you can download resources, such as information regarding practical tips for caregivers, you can share your caregiving tips (and receive tips from others), and you can connect with other people who are experiencing the same situation as you and your loved one.

Take care of yourself. Any family member who is actively involved in the care of the patient should also take care of herself. This means you should take a break from caregiving by asking another family member to take care of your loved one for a short while. In order to be helpful to your loved one, you need to stay healthy and happy, too. Keep your own life in balance. Do this by eating right, exercising daily, sleeping enough, and doing any activities you enjoyed before your loved one’s stroke.

















Comments
0 comment