views
In a global first, the British medical regulator has given the green light to a gene therapy aiming to cure two untreatable blood disorders – sickle cell disease (SCD) and beta-thalassemia.
The treatment for sickle cell disease and beta-thalassemia is the first to be licensed using the gene-editing tool Crispr, which earned its discoverers the Nobel Prize in 2020. This marks ground-breaking progress in managing two hereditary blood conditions, both stemming from gene errors related to haemoglobin.
It could be a game-changing technology for India which is known to have the highest prevalence of the disease – for both, thalassemia and SCD patients. However, typically it takes three to four years to bring the technology to India along with another challenge of high and unaffordable cost. According to media reports, the technology is expected to cost between $1.2 million (Rs 10 crore) and $1.7 million (Rs 15 crore).
Why does India need Crispr?
Data suggests that India has over two crore or 20 million patients with SCD and the largest number of children with Thalassemia major in the world — about 1.5 lakh with more than four crore or 40 million carriers of beta thalassemia trait.
Government estimates show that about 10,000-15,000 babies with thalassemia major are born every year and struggle to reach adulthood due to frequent blood transfusions, putting them at risk of iron overload, organ damage and critical blood-related infections such as HIV and Hepatitis C.
Patients with sickle cell disease experience the deformation of red blood cells into a sickle shape, leading to pain, anaemia, and organ damage. Thalassemia patients face anaemia and fatigue due to the insufficient production of haemoglobin, impacting oxygen transport. Such patients need frequent blood transfusions, in some cases weekly or fortnightly, to survive.
According to doctors in India treating these blood disorders, the country should immediately start trials to make the technology available.
“Approval of gene therapy in thalassemia and sickle cell anaemia is a great boon for these patients especially those who don’t have HLA-matched donors available,” JS Arora, general secretary at National Thalassemia Welfare Society & Federation, told News18.
While the cost will remain the biggest hurdle for Indian patients, he said the government should take effective measures to initiate clinical trials on this ‘urgently’.
Dr Chandrakanth MV, academic head and senior consultant, medical oncology and hemato oncology at Narayana Hospital in Howrah, said “given the current regulatory scenario in India pertaining to new drugs and therapies (their efficacy, trials, and patient safety), it will take more than three years for their availability and introduction in India”.
Why did the UK approve the technology?
The approval from UK’s regulator, the Medicines and Healthcare products Regulatory Agency (MHRA), comes after positive outcomes from clinical trials evaluating a single-dose intravenous infusion treatment.
This innovative therapy was created through collaboration between Vertex Pharmaceuticals in Boston, Massachusetts, and CRISPR Therapeutics, a biotechnology company based in Zug, Switzerland. The treatment, named Casgevy, uses a gene-editing tool.
In a trial for sickle-cell disease on 45 participants, Casgevy totally relieved 28 participants of agonising pain for at least one year post-treatment.
The researchers also assessed the therapy’s efficacy for a severe form of beta thalassaemia, typically managed with monthly blood transfusions. In this trial, 54 individuals received Casgevy, with 42 participating sufficiently to yield interim results. Among these 42 participants, 39 were free from blood transfusions for a minimum of one year, while the remaining three experienced a reduction of more than 70 per cent in their need for blood transfusions.
How does the tech work?
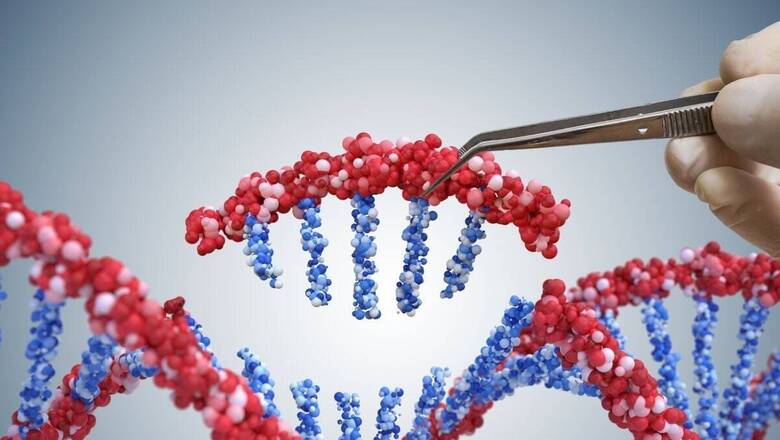
DNA is like the blueprint of our bodies and genes provide instructions for how our cells function. Gene-editing allows scientists to precisely manipulate this DNA. Errors in the genes responsible for encoding haemoglobin – a crucial molecule facilitating the transport of oxygen by red blood cells – lead to the development of sickle-cell disease and beta thalassaemia.
Doctors use Casgevy by taking blood-producing stem cells from the bone marrow of patients. Then, they use CRISPR-Cas9, a kind of molecular scissors, to edit the genes that carry instructions for making haemoglobin in those cells. This editing tool uses an RNA molecule to guide it to the right spot in the DNA, where it makes precise cuts.
In simple words, when Cas9 gets to the gene called BCL11A, which is the target of Casgevy, it cuts both sides of the DNA. Normally, BCL11A stops the creation of a type of haemoglobin that is usually only made in babies before they are born.
By changing this gene, Casgevy allows the body to make foetal haemoglobin, which is different from adult haemoglobin and doesn’t have the same defects in people with sickle-cell disease or beta thalassaemia.
Experts push for faster adoption of Crispr in India
Traditionally, the only permanent treatment option has been a bone marrow transplant, a procedure with rejection risks and dependency on a closely matched donor.
However, this gene-editing treatment has demonstrated its ‘first-of-its-kind’ status by successfully restoring healthy haemoglobin production in the majority of participants.
“By using cas technique – which doesn’t use a viral vector traditionally used for gene therapy – genetic code is modified and leads to cure of the two blood disorders,” Satya Prakash Yadav, director, pediatric haematology, oncology and bone marrow transplant at Medanta Hospital, said.
He said that usually, it takes three to five years before new therapies reach India. “In this case, cost is also going to be a barrier apart from availability.”
While gene editing is known to cause side effects in the later stages of life, including the risk of cancer, Yadav said “none reported in this trial so far which is good”. “However, side effects have to be looked at for the next ten years,” he added.
India has been actively integrating gene therapy and related protocols.
With 2019 guidelines from the Indian Council of Medical Research emphasising ethical considerations already, the Gene Therapy and Advisory and Evaluation Committee was also being set to oversee the proposed therapies.
“We need to recognise the potential of gene therapy amid a significant burden of genetic disorders, addressing technical risks and ethical challenges with a robust regulatory framework,” Dr Chandrakanth MV from Narayana Hospital said, adding that “as healthcare professionals, we strongly recommend expediting the introduction of new therapies”.















Comments
0 comment