views
Knowing When to Get a Tetanus Shot
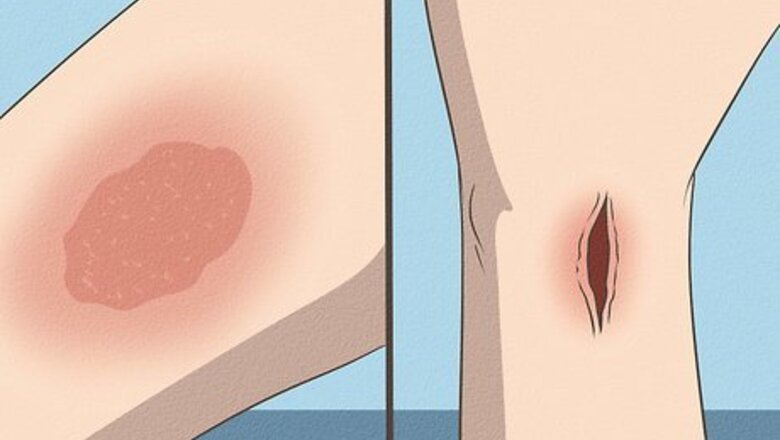
Get a tetanus booster shot after getting a deep or contaminated wound. Usually, the bacterial toxins enter the body through a break in the skin caused by an object contaminated with tetanus. If you have one or more of the following injuries or wounds that are prone to tetanus, get a tetanus booster shot. These include: Any wound visibly contaminated with soil, dust, rust, saliva, or horse manure. Puncture wounds. Objects that can cause these types of wounds include wood splinters, nails, needles, glass, and human or animal bites. Skin burns. Second-degree (partial-thickness or with blisters) and third-degree (full-thickness) burns are at higher risk for tetanus infection than first-degree (superficial) burns. Crush injuries that damage tissue by squeezing it between two heavy objects. They can also happen when heavy objects are dropped onto parts of the body. Wounds involving necrotic, or dead, tissue. This kind of tissue has no blood supply, increasing its risk for infection (along with severely compromised tissue). For example, areas of gangrene (dead body tissue) are at increased risk for infection. Wounds with foreign objects in them. Wounds that have foreign bodies, such as splinters, glass shards, gravel, or other objects in them are at higher risk for infection.

Get a tetanus shot if you’re not up-to-date on your vaccines. If you never received the first series of tetanus shots (primary vaccination series) or you're not sure when you had your last tetanus shot, go get a tetanus shot. Also, get a booster If you’re injured in any of the following ways: Your wound was caused by a “clean” object, but your last tetanus shot was over 10 years ago. Your wound was caused by a “dirty” object and your last tetanus shot was more than 5 years ago. A dirty, or contaminated, object has dirt/soil, saliva, or feces/manure on it, while a clean object does not. However, you can't necessarily know if an object has bacteria on it by looking at it. You're not sure if the wound was caused by a “clean” or “dirty” object and your last tetanus shot was over 5 years ago.

Get the shot while pregnant. In order to transfer tetanus antibodies to your baby, get a tetanus vaccine when you are between 27 and 36 weeks pregnant. Your doctor will likely recommend the inactivated Tdap (Tetanus, Diptheria, and Pertussis) vaccine during the third trimester of your pregnancy. If you have not had the Tdap vaccine before and don't have it during pregnancy, get vaccinated immediately after giving birth. Anyone else interacting with your baby also needs a Tdap vaccine at least two weeks before seeing them. If you get a dirty cut or wound while pregnant, absolutely get a tetanus booster shot.
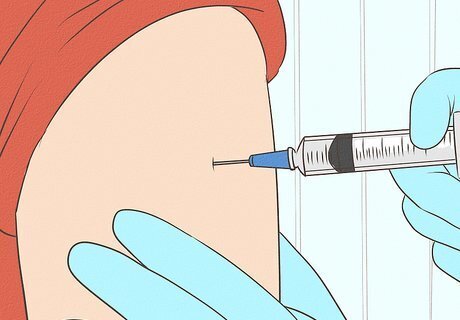
Get a round of tetanus shots to become immunized. The best way to "treat" tetanus is to prevent it in the first place. Several vaccines protect against tetanus. They are: DTaP. The diphtheria, tetanus, and pertussis (whooping cough) vaccine (DTaP) are usually given to babies at ages 2, 4, and 6 months, then again at 15 to 18 months old, and finally once more between ages 4 and 6. DTap is a very effective vaccine for small children. Tdap. Over time, protection from tetanus decreases, so older children need to get a booster shot. It has a full dose of tetanus and lower amounts of diphtheria and pertussis. All people between the ages of 11 and 18 are advised to get the booster, preferably around 11 or 12 years old. Td. If you're an adult, get a Td (tetanus and diphtheria) booster shot every 10 years to stay protected. Since some people may lose the protective antibody levels after 5 years, a booster vaccination is recommended if you get a deep, contaminated wound and haven't had a vaccination in more than 5 years, even if you’ve had the full round of childhood immunizations. Most people don't experience serious reactions to the vaccine, but there are a few common mild reactions. These include localized swelling, tenderness, and redness at the injection site, but these often clear up in 1-2 days.
Learning About and Recognizing Tetanus
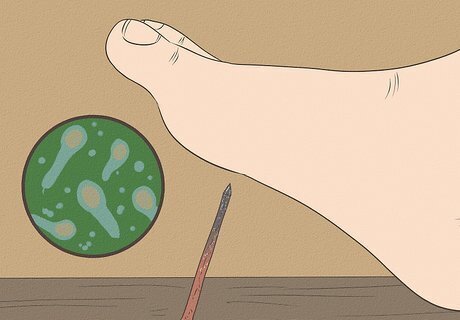
Learn how tetanus is contracted and spread. Tetanus is spread by bacterial spores that usually enter the body through a puncture. The spores make a powerful neurotoxin that can cause muscle spasms and stiffness. Tetanus is not, however, spread from person to person, unlike other vaccine-preventable diseases. Nearly all cases of tetanus occur when someone isn’t up to date on their shots. Tetanus is preventable with vaccines, so if you’re unvaccinated or haven’t kept up with your 10-year boosters, you are at a higher risk of tetanus. Complications from tetanus are highest among people who have not been immunized at all or in older adults with inadequate immunization in industrialized countries. You may also be at increased risk of tetanus after a natural disaster, especially if you live in a developing country.

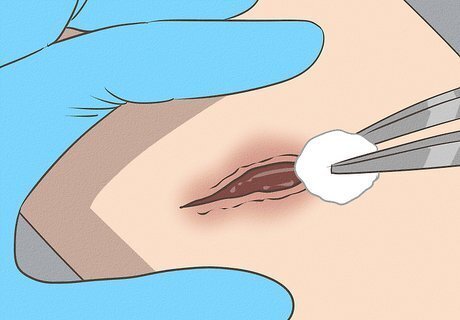
Disinfect your wounds to reduce your risk for tetanus. As soon as you get an injury or wound, wash your hands with soap and water, then clean and disinfect the area. If you delay disinfecting the new wounds by more than 4 hours, you increase the chances of tetanus infection. This is even more important if the wound was caused by an object that punctured the skin, which can force bacteria and debris deep into the wound, making it an ideal environment for the growth of bacteria. Pay attention to whether the object that caused your wound is clean or dirty to decide whether you need a tetanus booster.

Seek care if you develop tetanus symptoms. The incubation period varies from 3 to 21 days, with an average of 8 days. Tetanus severity is determined on a scale from I through IV. The longer it takes symptoms to appear, the more mild the disease is likely to be. The symptoms of tetanus (in order of appearance) include: Spasm of jaw muscles (commonly referred to as “lockjaw”) Stiffness of the neck Difficulty swallowing (dysphagia) Board-like rigidity of the abdominal muscles

Recognize other symptoms of tetanus. There are no blood tests that can diagnose tetanus, so it's important to pay attention to any symptoms. You may also notice fever, sweating, elevated blood pressure, or rapid heart rate (tachycardia). Possible complications include: Laryngospasm, or spasm of the vocal cords, which can make breathing difficult Bone fractures Seizures/convulsions Abnormal heart rhythms Secondary infections, such as pneumonia, as a result of prolonged hospitalization Pulmonary embolism, or blood clots in the lungs Death (10% of reported cases are fatal)
Treating Tetanus
Get medical attention. If you think or even suspect you have tetanus, seek medical treatment immediately. It's a medical emergency and you'll need to be hospitalized because tetanus has a high mortality, or death, rate (10%). In the hospital, you'll be given a tetanus antitoxin, like tetanus immune globulin. This will neutralize any toxin that hasn't already bound to your nervous tissue. The wound will be thoroughly cleaned and you'll get a tetanus vaccine to prevent future infections. Being infected with tetanus does not give you immunity from future infection. Instead, you'll need to get the tetanus vaccine to keep from getting it again.
Have a doctor determine your course of treatment. Since there are no blood tests that can diagnose tetanus, lab testing is not useful in the evaluation of the disease. Because of this, most doctors opt for aggressive treatment if infection is suspected, instead of taking a “wait and see” approach. Doctors base their diagnosis mainly on the symptoms and clinical signs that are present. The more severe the symptoms, the more rapid the course of action.

Treat the symptoms of tetanus. Since there is no cure for tetanus, treatments are directed at symptoms and emerging complications. Symptoms are treated with antitoxins; antibiotics given intravenously, by injection, or orally; and other drugs to control muscle spasms. Some of the drugs to control muscle spasms include sedatives from the benzodiazepine group (like diazepam (Valium), lorazepam (Ativan), alprazolam (Xanax), and midazolam (Versed). Antibiotics are not generally effective against tetanus, but they may be prescribed to keep the Clostridium tetani bacteria from reproducing. This can help slow the production of toxins.















Comments
0 comment